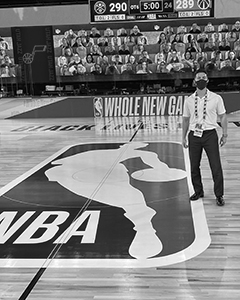
In this issue, we talked to Dr. Bryan Murtaugh of MedStar National Rehabilitation Network in Washington, D.C. Dr. Murtaugh works with the Washington Wizards and has been transitioning from a normal season to the National Basketball Association (NBA) "bubble" during COVID-19. The following article is based on his experience as of late July 2020.
 Bryan Murtaugh, MD, FAAPMR
Bryan Murtaugh, MD, FAAPMR
Director of Sports Medicine
MedStar National Rehabilitation Network
Working as a team physician in professional sports is never routine, even after five years with the Washington Wizards. Yet I had grown comfortable with my responsibilities focused on handling many of the primary care needs for the athletes. Then, COVID-19 struck the world, causing widespread shutdowns, including suspension of the NBA season in March. However, in May, I learned there was the possibility for a resumption of the season, albeit much different than any other season.
As plans developed, our focus turned to getting our players back to training and competing safely. This involved quite a bit of coordination of care, numerous meetings and memos, consultations with our infectious disease specialist and discussion of our policies and procedures with the entire medical staff and organization.
Planning to compete in the COVID-19 era was a collective effort between the NBA executives, medical staff from around the league and the players to ensure the transition to playing was safe. Each team's practice facility required plans for temperature and symptom screening, social distancing, mask requirements, disinfection and sanitization procedures and coordinated scheduling of individual drills rather than team practice. In the weeks leading up to traveling to enter the "bubble" in Orlando, we had to test the whole travel party every other day. After a period of quarantining in our hotel rooms, this transitioned to daily testing to confirm that we remained COVID-19 negative. Prior to leaving our hotel rooms every morning, we were required to take our temperature, oxygen saturation and complete a COVID-19 screening questionnaire. All of this information was uploaded to a wristband that allowed us to access various checkpoints throughout the campus. Also, a sensor was attached to our credentials to ensure we were maintaining social distancing.
For the first several weeks there were five team physicians across the 22 team that made the trip to Orlando. This initial period involved not only taking care of the players from across the league, but also included developing the protocols and navigating the difficulties of delivering care within the confines of the "bubble." Simple things we take for granted as easy and efficient in our everyday practices were a challenge, requiring a high level of coordination. There was no "playbook" for what we were doing, so figuring out how to get things done with the other team physicians was one of the most challenging but enjoyable experiences. We had different primary specialty training, but we worked well together through the early struggles. More physicians entered "the bubble" in the following weeks and I admired the dedication that each of them demonstrated. It was good to see another physiatrist there, Dr. Steve Yoon. I believe having a presence there helps move physiatry forward in terms of other specialties understanding what we as physiatrists do and what value we bring to patient care.
While I'm doing my part for my patients in the bubble, I'm proud to see what my fellow physiatrists are doing. I know my colleagues who have transitioned much of their practice to telehealth - not an easy feat when it's totally different from what we're used to! Or those who have been on the frontline with testing or involved with musculoskeletal clinics attached to their emergency rooms. COVID-19 has presented challenges to all of us. However, physiatrists are skilled in being able to assess needs and adapt to change. It's been inspiring to see how my colleagues have stepped up to the challenge. We've seen that COVID-19 can cause severe debility in our patients, and at the heart of physiatry we've always been involved with helping patients restore their function.
At the same time, physiatrists are always finding ways to keep our patients active. From a sports medicine perspective, we've had many patients that have had to stay home without access to a gum because of the pandemic, meaning we have to find unique ways to keep our patients active and healthy. Simultaneously, they may be doing new exercise routines at home and sometimes these transitions can put them at risk for injury; therefore we are well qualified to provide guidance with this.
My advice for fellow sports medicine physiatrists? Planning is key. Regarding team sports coverage, it is paramount to understand how to best minimize the risks of infection, whether it be wearing masks, exercising social distancing, performing temperature and symptom screen checks at every access point, disinfection protocols and creating pods at any practices. It's just as important to understand what resources you have, including testing capabilities and personnel for counseling on isolation, contact tracing and quarantining. Also, protocols should be developed for clearance to return to play for those athletes who had a positive test. All of this, to succeed, takes a high level of coordination of care, open communication and planning upfront with the rest of your medical staff.